At the Quality Institute, we have long championed alternative payment models that support high-quality and comprehensive primary care. We have another opportunity to improve the health of our state now that the CMS Innovation Center has selected New Jersey to participate in a potentially transformative model of care.
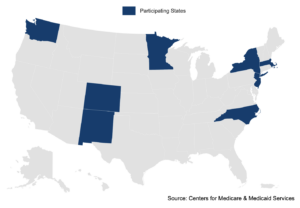
New Jersey is one of just eight states selected for Making Care Primary, a model that is scheduled to run for ten and half years, with six months for planning, making it the longest model ever tested by the Innovation Center. The time span recognizes the importance of comprehensive primary care as the foundation of a well-functioning health care system — and the vast changes we need to get us there. The model is open to primary care practices, including Federally Qualified Health Centers, if they see a minimum number of Medicare patients.
An exciting element is that New Jersey’s Medicaid program will be an important partner with participating primary care practices, health plans, and community-based organizations, a recognition of the need to connect people to social services to further their wellbeing. The practices also will be encouraged and supported to work with behavioral health providers within and outside their practices to deliver better integrated care.
In designing the model, the Innovation Center reflected on lessons learned from previous primary care innovation models, including learnings from New Jersey, a participating state in earlier models. A goal now is to help smaller practices or those with limited experience in alternative payment models to set up the needed infrastructure and move toward comprehensive care. CMS leaders found that their models needed to be more inclusive to all types of primary care practices to “meet them where they are.” In that regard, the model enables practices to enter one of three tracks with corresponding payments and requirements.
CMS leaders also learned that all payers — Medicare, Medicaid, commercial — must be involved for a practice to successfully transform. They also found that the process will take far longer than prior model lengths to transform and test a model. The Making Care Primary model puts emphasis on providing the practices with tools to support their transformation, such as data on specialists in three high volume, high-cost areas where primary care connectivity and coordination is essential to patient outcomes and costs.
The United States has historically under-invested in primary care compared to other high-income countries. After listening to the information sessions to date, to me the overarching purpose is to move primary care away from a fee-for-service model that doesn’t pay enough — and isn’t designed to reimburse clinicians to work as a team and to spend enough time with their patients. The model changes payments, over time, to invest in practices upfront and provides a predictable revenue stream so practices can take on a manageable number of patients and ensure they receive timely and well-coordinated care. The model also enables primary care practitioners to meet the wider health needs of their patients.
If your organization would like to submit a letter of intent, here is the link. At the Quality Institute, we view Making Care Primary as an unprecedented and valuable opportunity for New Jersey. Please help us spread the word — and consider participation if your organization is eligible. And keep working with us in other ways to continue the push for equitable, high quality primary care for everyone.